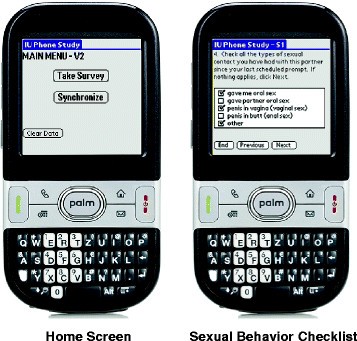
Several software packages, such as the Purdue 23 24 Momentary Assessment Tool, MyExperience, and Considerations for Inpatient and Outpatient Samples. De- ClinTouch (as well as several home-made programs) spite the successful application of mobile assessment in have been used for programming experience sampling pro- schizophrenia research. Nov 18, 2013 Purdue Momentary Assessment Tool (Weiss et al., 2004). The study, participants were debriefed and compensated. Interpersonal Support Evaluation List (ISEL). The PDAs were programmed using a modified version of the Purdue Momentary Assessment Tool version 2.1.2. 27 The EMAc questions used visual analog scales and box-checking formats to collect all responses. Initial pilot work demonstrated that this population had difficulty remembering options between screens and often did not scroll to the next screen without prompting. Feb 10, 2013 The PDAs were programmed to administer four electronic interviews per day for seven days. A modified version of the Purdue Momentary Assessment Tool version 2.1.2 (Weiss et al., 2004) was used in the PDA programming. This tool provides time stamps for all data entries and permits responses only within a 15-minute period following an alarm signal.
July 26, 2017 |
A Purdue University precision innovation developed for brain tumor surgery is being expanded to provide medical professionals with a rapid, robust supplemental assessment tool to more efficiently preserve, analyze and remove identified cancerous tissue and increase patient survival rates.
The technology was developed out of the Aston Lab in Purdue’s College of Science, headed by Graham Cooks, the Henry B. Hass distinguished professor of analytical chemistry. Valentina Pirro, a research scientist in Purdue’s Department of Chemistry, was also instrumental in the technology’s development.
The team’s morphologically friendly mass spectrometry imaging technique could determine if microscopic cancerous tissue is still present in a sample and thus provide more information to influence a surgeon’s decisions regarding further tissue removal.
Pirro says other mass spectrometry techniques have limitations.
“Mass spectrometry can identify and measure molecules within a tissue by measuring a signal that relates to the mass and structure of the molecule. It can be used in cancer diagnostics because it’s able to monitor the differential distribution of lipids or malformed metabolites that distinguish normal and cancerous tissue,” she says. “With some form of mass spectrometry imaging, the chemicals or solvents used in the process can often destroy the tissue sample. Essentially, you have one shot at getting the data and then the sample is gone.”
Cooks and his research team have developed a morphologically friendly method for tissue imaging that can be used to perform Desorption Electrospray Ionization Mass Spectrometry (DESI-MS).
“Our method allows researchers to choose solvent combinations that don’t affect the morphology, or form, of the tissue. This means the tissue’s native structure is preserved and after the experiment you’re able to take your tissue and stain it or use it for other experiments to retrieve complementary chemical information,” Pirro said. “The analysis is extremely simple and straightforward, because we can analyze tissue sections or smears with no sample preparation and then validate our results with standard histopathology. Essentially this solvent is used as a spray that is directed onto a small area of a sample and extracts molecules contained within. We can run an image by simply moving the spray right on top of a tissue section or smear.”
This assessment can be completed quickly while in the operating room, without interfering with the surgery, Pirro added.
“We were able to modify a commercial DESI-MS instrument so that it sits on top of a cart as a standalone system and can be easily wheeled in the operating room when needed. Once a surgeon resects a small biopsy, we can smear it on a glass slide and analyze it as is. After a few minutes we can tell the surgeon if the tumor is still present in the tissue sample and estimate the percentage of infiltration,” she says. “By adding these objective measures, we are hoping that the surgeon will be guided in the resection and make fast decisions on whether or not to remove more tissue.”
Pirro says that preoperative MRI images are typically used to help guide surgeons; however, they are limited.
“Preoperative MRI images don’t always precisely translate to the area of surgery,” she says. “Additionally, there may be high infiltration of the tumor beyond what the MRI image is able to see. These limitations can cause difficulty in safely removing as much of the tumor as possible.”
The technical challenges for brain tumor surgery and treatment applications helped led the research team to this expanded use of the technology.
“Brain tumors are specifically complicated because they infiltrate into the brain and don’t make clear borders,” Pirro says. “In order to make sure the patient has the highest chance of survival, it’s imperative that as much cancer tissue as possible is removed while trying to minimize neurological damages.”
The technology is currently being used in preclinical settings.
“We have completed studies on a lot of tissue samples to confirm that we are able to get valuable diagnostic information. We are currently using the technique in the operating room in preclinical assessments where we perform our experiment without influencing the surgical practice itself,” Pirro says. “We have completed 18 different surgeries to show that the assessment is feasible, rapid and robust. Additionally, we have been able to identify tissue highly-infiltrated with tumor even when the MRI images may say otherwise.”
Pirro says the next step for the technology is a clinical trial.
“Through a clinical trial the technology could influence the decision strategy. Ideally you would compare surgeries done with and without this technology and see if there is an improvement in the survival rate,” she says. “We imagine a company licensing this technology to take these next steps before eventually bringing it to market and provide this supplemental tool to surgeons everywhere.”
The Purdue Research Foundation’s Office of Technology Commercialization has patented the technology and it is available for license. For information, call 765-588-3470 or email innovation@prf.org.

Original: http://bit.ly/2hnBQBI
Purpose
The Purdue Pegboard aids in the selection and rehabilitation of employees for various types of manual labor by measuring 2 types of dexterity:
- Gross movements of the fingers, hands and arms.
- Fine fingertip dexterity necessary in assembly tasks.
Area of Assessment
CoordinationDexterity
Cost
Not FreeCost Description
$110-150Diagnosis/Conditions
- Parkinson's Disease + Neurologic Rehabilitation
Populations

- The Purdue Pegboard Test is a rectangular board with 2 sets of 25 holes running vertically and 4 concave cups at the top. Small metal pegs are placed in the cup on the side being tested, with subjects asked to remove the pegs and place them vertically in the holes as rapidly as possible. The number of pegs placed in 30 seconds is scored.
- The original application for the test was for testing the dexterity of industrial workers. It has since been used for testing of dexterity testing within various populations in the clinical setting, including children and adolescents.
- The test takes about 30 seconds per activity for a total of 5-10 minutes including instruction. The test administrator compiles 5 separate scores from the complete test procedure, one for each battery:
1) Right Hand (30 seconds)
2) Left Hand (30 seconds)
3) Both Hands (30 seconds)
4) Right+Left+Both Hands (This is not an actual test, but a mathematical sum calculation)
5) Assembly (60 seconds)
(Lafayette Instrument Company User’s Manual, 2002)
Equipment Required
- Purdue Pegboard Test
- Instruction Manual
- Test Board
- Pins, Collars, Washers
- Score Sheets
- At least one testing table approximately 30 inches tall. The subject must be seated throughout the administration of the test.
- Stopwatch
Required Training
Reading an Article/ManualAge Ranges
Adolescent
13 - 17
yearsElderly Adult
65 +
yearsInstrument Reviewers
References from the Parkinson’s disease population by Jeffrey Hoder, PT, DPT, NCS and the PD EDGE Task Force of the Neurology section of the APTA
ICF Domain
Body FunctionProfessional Association Recommendation
Recommendations for use of the instrument from the Neurology Section of the American Physical Therapy Association’s Multiple Sclerosis Taskforce (MSEDGE), Parkinson’s Taskforce (PD EDGE), Spinal Cord Injury Taskforce (PD EDGE), Stroke Taskforce (StrokEDGE), Traumatic Brain Injury Taskforce (TBI EDGE), and Vestibular Taskforce (Vestibular EDGE) are listed below. These recommendations were developed by a panel of research and clinical experts using a modified Delphi process.
For detailed information about how recommendations were made, please visit: http://www.neuropt.org/go/healthcare-professionals/neurology-section-outcome-measures-recommendations
Abbreviations: | |
HR | Highly Recommend |
R | Recommend |
LS / UR | Reasonable to use, but limited study in target group / Unable to Recommend |
NR | Not Recommended |
Recommendations Based on Parkinson Disease Hoehn and Yahr stage:
I | II | III | IV | V | |
PD EDGE | LS/UR | R | R | R | LS/UR |
Recommendations for entry-level physical therapy education and use in research:
Students should learn to administer this tool? (Y/N) | Students should be exposed to tool? (Y/N) | Appropriate for use in intervention research studies? (Y/N) | Is additional research warranted for this tool (Y/N) | |
PD EDGE | No | No | Yes | Not reported |
Considerations
Purdue Momentary Assessment Tool Box

Parkinson’s disease: Strong psychometrics. It is valid and reliable. It has been used in medication trials (Tan, 2003), post neurosurgery (Pal, 2000) and to measure dexterity during off times in PD (Brown, 1998). It was used to test dexterity during dual task performance (Proud, 2010). Correlated strongly to UPDRS total and motor (Proud, 2010). Dexterity decreases with increased severity of disease. Pegboard scores best correlated with bradykinesia and loss of dopamine per PET scan (Vingerhoets, 1997).
Do you see an error or have a suggestion for this instrument summary? Please e-mail us!
Teacher Assessment Tool
Normative Data
(Tiffin, 1948)
Normative data was established on factory workers who performed manual tasks for their occupation.

Bibliography
Brown, R. G. and Jahanshahi, M. (1998). 'An unusual enhancement of motor performance during bimanual movement in Parkinson's disease.' J Neurol Neurosurg Psychiatry 64(6): 813-816. Find it on PubMed
Pal, P. K., Samii, A., et al. (2000). 'Long term outcome of unilateral pallidotomy: follow up of 15 patients for 3 years.' J Neurol Neurosurg Psychiatry 69(3): 337-344. Find it on PubMed
Proud, E. L. and Morris, M. E. (2010). 'Skilled hand dexterity in Parkinson's disease: effects of adding a concurrent task.' Arch Phys Med Rehabil 91(5): 794-799. Find it on PubMed
Tan, E. K., Ratnagopal, P., et al. (2003). 'Piribedil and bromocriptine in Parkinson's disease: a single-blind crossover study.' Acta Neurol Scand 107(3): 202-206. Find it on PubMed
Vingerhoets, F. J., Schulzer, M., et al. (1997). 'Which clinical sign of Parkinson's disease best reflects the nigrostriatal lesion?' Annals of neurology 41(1): 58-64.